Response to recent NY Times article about Crestor and
statin use. (posted 3/31/10) Recently the NY Times published an article entitled
“ Risks Seen in Cholesterol Drug Use in Healthy People” (http://www.nytimes.com/2010/03/31/business/31statins.html
) . The article raises questions about whether or not healthy patients with elevated high sensitivity
C-reactive protein (hs-CRP)and other cardiovascular risk factors should be treated with statin medications even if their LDL
cholesterol is normal. The article raises questions about whether or not statins are safe to be taken as preventive medicines.
The debate here should not
be about whether or not statins work, nor on whether or not the drug has been proven to work on younger people. Statins do
work, ask any young patient with familial hyperlipidemia, who would normally die by the age of 30. What this debate should
center on is why; despite the introduction of statins is heart disease the number one cause of death in the US? It is because
the cause of this disease, abnormal lipoproteins, the carriers of cholesterol are not measured by standard cholesterol tests.
Most patients who have heart disease do not have elevated LDL (bad ) cholesterol. They do , however have elevated lipoproteins(specifically
Apolipoprotein B(ApoB)). Once Apo B lipoproteins start the process of atherosclerosis, inflammation begins,
and tests like hs-CRP become elevated. Rather than wait for this to happen, simply indentify and treat the cause, the Apo
B lipoproteins with statins and other drugs along with lifestyle changes when appropriate. Many cholesterol
disorders are genetic, and for these patients drugs offer the only option. For many obesity, diabetes, and poor dietary and
exercise habits contribute to the abnormal Apo B lipoproteins. Simply testing for elevated levels of Apo
B lipoproteins would identify many at risk long before hs-CRP was elevated. Statins
do increase risk of diabetes, and those patients with diabetes benefit the MOST from statins. The cause of this has not been
determined. Niacin increases diabetes risk, and again, those that benefits most on niacin are diabetics.
Niacin is a natural b vitamin. The first statin came from the same yeast that produced penicillin. Treating with statins does
more than simply preventing death from heart disease; it prevents strokes, especially in women. Preventing a nonfatal stroke
is one of the best things one can ever do. There is much we still do not know, but there is much we do know, and have known
for a very long time. For more that 50 years now it has been clear that Apo B lipoproteins cause atherosclerosis, yet many
insurance companies still think testing for lipoproteins is "experimental". Medicare allows this test, and recognizes
its value. Hs-CRP is variable and many patients who have elevated CRP , might not one month later. If it remains elevated
over time it does signify cardiovascular risk. Just check the lipoproteins and for many they would never get to a point where
hs-CRP and statins are needed. If we found our younger patients at risk there would be more time to attempt
correction of these abnormalities with lifestyle changes. The problem is not with the FDA, nor with pharma companies that
manufacture statins. The problem is with our ever expanding waistline, and reversing this trend. With obesity comes increased
Apo B lipoproteins, along with high blood pressure, diabetes. This drives the process of atherosclerosis. Statins are one
small piece of the puzzle, but when used properly, in the right patients, those with elevated lipoproteins, can be helpful.
You cannot prevent a problem if you do not know whether or not the cause is present. If more patients where checked for abnormal
Apo B lipoproteins then statins would be used more appropriately, and many would be identified and perhaps
treated with lifestyle changes long before statins were required. How do you check lipoprotein levels? Either my measuring Apo B levels in the blood. Apo B is a surrogate for
LDL cholesterol particles. One can also measure LDL particle levels directly, and this method also includes traditional cholesterol
values along with additional information about what the cause of the underlying cholesterol problem may be. Simvastatin (generic
Zocor) Highest Dose Linked to Muscle Problems (Posted 3/21/10)Recently the FDA released a drug safety
communication about the increased risk of rhabdomyolysis and myositis (muscle breakdown and inflammation) at the highest dose
of simvastatin(formerly Zocor) when taken at the highest dose of 80 mg when compared to the 20 mg dose.
While those of us in the cholesterol community , lipidologists and preventive cardiovascular cardiovascular
specialists have suspected this to be the case for a while now, this confirms our concerns that the potential benefits of
this high dose are significantly outweighed by the risk. Most of the clinical data supporting the benefits of simvastatin
in lowering cholesterol in patients at risk for heart disease and reducing risk of cardiovascular events have been with doses
of the drug between the 20-40 mg dose. When LDL cholesterol (bad cholesterol) is lowered more then about 30%
these benefits are demonstrated. It takes somewhere between 20-40 mg of simvastatin to achieve this reduction, and this is
the dose most patients use as prescribed by their physicians. When cholesterol targets have not been achieved often statin
doses are increased. The expected additional increase in cholesterol lowering when simvastatin dose is
doubled from 40 to 80 mg (the highest dose) is only approximately 5-6 %. This minimal increase in cholesterol lowering is
accompanied with an increased risk of muscle side effects. So why would one use the 80 mg dose of simvastatin?
In most cases when 40 mg of simvastatin is not effective, doctors either add a second drug, or change the simvastatin to a
more potent statin such as atorvastatin (Lipitor) or Rosuvastatin (Crestor). Simvastatin however is generic
and costs less , and many managed care organizations and prescription benefit companies require that patients
have been tried on the highest dose of zocor before they will approve use of a non-generic statin. We do not use the
80 mg dose of simvastatin because we do not feel the risk outweighs any potential benefit, and perhaps now, with this new
information patients will not be unnecessarily treated with this dose prior to being switched to a drug that is more appropriate
for them. If you are taking simvastatin 80 mg you should discuss the use of this drug
with your health care practitioner. Many patients do take this and tolerate it well. For some it is the only drug they can
afford or can tolerate. Awareness of this data , however , is important for both patients
and health care providers to consider when making treatment choices. ACCORD Trial Update (posted 3/17/2010) This
week at the American College of Cardiology Meetings in Atlanta GA, the results of the ACCORD Trial were released. ACCORD stands
for “The Action to Control Cardiovascular Risk In Diabetes”. This study had three parts, one investigating control
of blood sugar, one investigating the control of blood pressure and the third investigating the control of lipids (cholesterol
,triglycerides etc) all in diabetic patients. The results of the diabetes study were reported last year showing no benefit
in treating diabetic patients to very low blood sugars. The blood pressure was reported this past week, showing no benefit
other than perhaps a reduction in stroke risk when diabetics are treated to lower blood pressure targets.
Finally on Sunday of this week the long anticipated results of the lipid study were released. These patients were diabetic
and all were given a statin medication (Simvastatin) at a dose of between 20-40 mg. Half of the patients were given in addition
to the simvastatin a second drug called fenofibrate. This drug lowers triglycerides, raises the good HDL cholesterol and in
some patients lowers the bad LDL cholesterol. The thinking was that in diabetic patients there would be an additional benefit
of treating cholesterol and triglycerides more aggressively. The
study results showed a trend towards benefit in the group that got the second drug, but this was NOT statistically significant,
and hence the results were reported as neutral. There was also a trend towards worse outcomes in the women who got the fibrate,
but again, this was NOT statistically significant. In looking at subgroups of patients, the one type that seemed to improve
on the dual therapy was those patients with low HDL (good cholesterol) and elevated triglyceride levels. What does this mean for patients? First, fibrates are safe drugs and can be used
in combination with statin medication if needed. They are excellent drugs for lowering high triglycerides levels, and can
be used in addition to statin medications to further lower LDL cholesterol and levels of lipoproteins (the carriers of cholesterol).
Fibrates should probably be reserved for those patients with low HDL cholesterol and elevated trigyclerides (both components
of something called metabolic syndrome) and often associated with obesity, high blood pressure and abnormal blood sugar, BUT
in diabetic patients already on a statin if the HDL cholesterol and Triglycerides are normal, probably will not yield additional
cardiovascular benefit. If you are taking a fibrate (fenofibrate,
tricor, gemfibrozil, trilipix, lipofen, etc) do not stop it on your own. Contact your physician and make an appointment to
discuss the role of this drug in your lipid and cardiovascular prevention therapy . Diabetes and Walnuts:potential cardiovascular benefits: posted 2/22/2010 This week at the American College of Preventive Medicine, where I chaired a symposium
on "Cholesterol and Blood Pressure Guidelines" a very interesting research study was reported. The preventive medicine
group at Yale University presented data showing that diabetic patients who supplemented their diets with walnuts had an improvement
in the function of their arteries (called endothelial function). Often patients with heart disease or risk factors for heart
disease (such as obesity, high blood pressure, abnormal cholesterol or erectile dysfunction) have abnormalities in endothelial
function long before they exhibit signs of cardiovascular disease. The investigators also looked at changes in total and LDL
(bad) cholesterol, showing a non-significant trend towards better cholesterol levels, but based on statistics reported the
levels as the same in each group. There were no changes in sugar control blood pressure and most importantly weight.
The patients were given 56 grams a day of walnuts. The fact that the patients did not gain weight suggests that health supplements
such as walnuts may be filling and decrease additional food intake. While the results are encouraging, it is important to
recognize that endothelial function is not a test that is done in most offices, and is used at this time almost exclusively
for research purposes. In addition, measuring endothelial function has not been shown to improve cardiovascular outcomes.
Since it does correlate with increased risk of cardiovascular events , improving it seems to be a good thing. Walnuts contain
increased amounts of Omega 3 fatty acids, most often consumed from fish . Other nuts, however , have also been shown
to help diabetics such as almonds (which may improve blood sugar levels). Heathy snacks such as walnuts and almonds (non salted
and non sugared) are reasonable for all patients, and may particularly benefit diabetics. For a complete review of this presentation
see Nancy A. Melville's article on theheart.org http://www.theheart.org/article/1049183.do. Statins and Diabetes: Posted 2/18/2010 Yesterday a study was released in the British Journal LANCET.
This study was a Meta-analysis (a study that reviews or combines many other studies into a larger group). The investigators
reviewed 13 large studies done with drugs in the statin class used for lowering cholesterol. The studies needed to include
more than 1000 patient and had to be longer than one year. Over all they looked at more than 90,000 patients.
When all the different types of statins were grouped together, those on statins had a 9% increased chance of developing
diabetes as compared to those not taking statin medication. While the overall group met statistical significance, when the
statins were stratified by specific drugs, the only medication that met statistical significance was Rosuvastatin (Crestor).
This is in line with the results of the JUPITER Study, which demonstrated similar trends for this drug. What is important to note about this study was that the beneficial impact of
statins on reducing cardiovascular disease outcomes is not reduced, and in many sub-studies the groups of patients that benefit
the MOST from statins are diabetic patients. Other drugs that lower cholesterol have also been shown to worsen blood sugar,
most notably NIACIN. Should statins
be avoided in diabetic patients? ABSOLOUTELY NOT. In fact, diabetic patients are one group that should be taking statins .
What about a “pre-diabetic” patient? Should statins be avoided in this group? Again I would say no . If Cholesterol
and Lipoprotein lowering is indicated, then statins should be used as per our current guidelines. If pre-diabetes exists,
aggressive life-style modification is still the gold standard here, including weight loss , diet and exercise. Diabetic and Pre-diabetic patients taking statins should NOT stop them, and if
they have questions should discuss with their physician.
ARBITER 6 HALTS Study Update Zetia and Niaspan Recently I attended the American Heart Association Meetings
in Orlando Florida. Presented at the meeting were the results of the ARBITER 6 HALTS study. This was a study comparing two
different drugs ADDED on to Statin therapy (such as Lipitor, Zocor etc). In patients with pre-existing heart disease with
low -normal HDL (good cholesterol) levels. Both groups of patients started with VERY low LDL cholesterol levels (less than
100) and were given either Niacin (Vitamin B3) at very high doses (2000 mg a day) or Zetia . The study was a small study and
was designed to look at thickness of the lining of the carotid arteries in the neck. The study was NOT designed to look at
heart attack, stroke or other cardiovascular events. The study was stopped early (for no clear reason as safety was not and
issue for either drug) . The results showed that the progression of plaque in the neck was delayed with both Zetia and Niacin
(the drug was a long acting version of niacin called Niaspan), with Niaspan actually causing some regression of the plaque.
Despite what the investigators speculated in the article ( and they were strongly chided by other specialists for these remarks)
there were no “negative “ effects of Zetia. It has been well know for a while now that Niaspan can cause regression of
plaque in neck arteries as well as perhaps in the arteries around the heart, however no study has been able to show that regression
of plaque is associated with a reduction in heart attack, stroke or death. The Niaspan was better at raising HDL cholesterol
than the Zetia, and studies with zetia have already shown that is does not cause regression of plaque when added to a statin
medication. Statin
medications have been well documented to reduce risk of heart attack and stroke, however several studies with statins have
shown either no change in carotid plaque or only delayed progression , just like Zetia in this study. So what does the study tell us? Not
much that we already didn’t know before hand! Both Niaspan and Zetia are excellent drugs to add on to statins to further
lower LDL cholesterol. In patients with pre-existing heart disease and low HDL cholesterol, Niaspan should probably be the
next drug added to a statin . Niaspan is often difficult for some to tolerate, can cause flushing, can worsen peptic ulcer
disease , can increase blood sugar and perhaps exacerbate gout. Neither Niaspan or Zetia should be used on their own unless
Statins cannot be used first. If you are taking Zetia DO NOT STOP IT. There is no reason to. If you have heart disease, low HDL cholesterol and
are already on a statin, Niaspan MAY be indicated but not in everyone, as you may not need it or may not be able to take it.
If you
need to discuss this further please schedule an appointment with me to discuss this further. Dr Underberg Cholesterol and Pregnancy Concerns for Mother AND Child
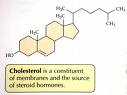
The story of cholesterol and pregnancy
is a very interesting one. Cholesterol is an important building block for all cells in our body. We require cholesterol for
cell membrane structure and function, and cholesterol serves as a precursor to many other substances such as hormones. It
is important for brain development and required by the developing fetus for normal gestation. During gestation many changes
take place that impact lipid and lipoprotein levels. There is a trend towards insulin resistance (pre-diabetes), accompanied
by changes in proteins and enzymes that control triglyceride and VLDL (very low density lipoprotein) metabolism such as lipoprotein
lipase, which causes an increase in triglyceride levels and VLDL particles. There is an increase in the
enzyme hormone sensitive lipase , which also contributes to some of these changes, and a reduction in hepatic lipase. This
is induced by increasing estrogen levels, and along with increased production of a protein called apolipoprotein A1, leads
to an increase in HDL (high density lipoprotein) levels. Thus the typical trend during pregnancy is for
an increase in LDL (low density) cholesterol, an increase in triglycerides, and an increase in HDL cholesterol. These changes in many women are physiologic
and minimal. For a woman with gestational diabetes they can lead to severe elevations in triglycerides in the third trimester,
which in some cases may necessitate hospitalization. The increase in cholesterol and VLDL particles, until recently has been
thought to be of no long term danger to the mother. As most cholesterol lowering medications are either pregnancy category
D or X (Dangerous), and should not be used during pregnancy, treating cholesterol disorders or women with very high cholesterol
during pregnancy has been thought to be more dangerous than the consequences. A recent article published in Current Opinion in Lipidology in 2009, reviews the data regarding
women with very high cholesterol levels from genetic causes (Familial Hyperlipidemia) (otherwise known as FH). Women with
FH have very high cholesterol levels from birth, along with a family history of early or “premature heart disease”.
In the most severe form, these patients often die in the second or third decades of life from cardiovascular causes. In a
less severe form (heterozygous FH or HetFH) the heart disease becomes symptomatic in the 4th or 5th
decade of life. While a 9 month hiatus from treatment for these women may not significantly affect long
term heart disease risk, the potential long term effects on the fetus, being exposed to very high cholesterol levels that
actually worse during the pregnancy is only now beginning to be understood. Studies done from autopsy studies in young children who die from other causes, combined
from accumulating evidence from animal studies suggest that this in-utero exposure to elevated cholesterol levels increases
the likelihood that early markers of atherosclerosis will be present in the offspring of mothers with FH. Therefore maternal
cholesterol levels even for the 9 months of pregnancy may impact future cardiovascular risk status of the child. What does this mean for treatment? Currently
there is only once class of lipid lowering medications that can be used safely during pregnancy, bile acid sequestrants. They
are pregnancy category B. This class of drug is not ideal, however, as it can raise triglycerides. As this is a concern as
pregnancy progresses, I does not represent a reasonable option for most throughout the full term of gestation. We must, therefore,
aggressively promote the importance of diet and lifestyle in non-pregnant female as not only important for maternal well being
but also for the offspring as well. During pregnancy, women are often told not to worry as much about diet. This may need
to change, and especially in those women with FH, or other cholesterol disorders, perhaps seeing a lipiodolgist (cholesterol
specialist) along with a nutrition specialist with expertise in both lipids and pregnancy would be reasonable. Finally, there
is always the possibility of new pharmacologic interventions being developed, however, clinical trials testing safety in pregnancy
would be very difficult to conduct. References1.Pregnancy
in women suffering from familial hypercholesterolemia: a harmful period for both mother and newborn? Current Opinion in
Lipidology 2009, 20:484–490 2. Lipoprotein metabolism and vascular complications in pregnancy.
Clin. Lipidol. 4(1), 91–102 (2009) 3. Influence or maternal
nutrition on the metabolic syndrome and cardiovascular risk in the offspring . Clinical Lipidology (2009)
4(2). 145-158
What does the new Crestor indication mean? Today
the FDA approved a new indication for the Statin Crestor (Rosuvastatin). In addition to its prior indications to lower cholesterol,
triglycerides and to delay the progression of atherosclerosis, it is now approved for primary prevention (patients with NO
history of heart disease or stroke) with normal LDL cholesterol and elevated high sensitivity C-Reactive Protein (hs-CRP)
(>2 mg/dl) in men >50 years of age and women >60 years of age WITH additional
risk factors for heart disease (low HDL cholesterol, hypertension, family history of premature heart disease or smokers).
The recommendations were based on the results of the JUPITER Trial (Justification
for the Use of statins in Prevention:
an Intervention Trial
Evaluation Rosuvastatin).
It is important to remember
that this study looked at a large number of patients over several years. Over 90,000 patients were screened so as to obtain
the necessary number of patients who qualified with normal LDL cholesterol levels and elevated hs-CRP levels. More than half
of the patients enrolled in this study had hypertension, and were overweight. The entry level blood sugars were in the upper
range of normal. In addition, many of these patients had elevated levels of apolipoprotein B, a marker of increased cardiovascular
risk. Hs-CRP levels are elevated
in patients with inflammation related to atherosclerosis, but are also elevated for many other conditions that cause inflammation.
A simple cold, ankle sprain or dental infection can all cause an increased hs-CRP level. When evaluating 18000 patients over
several years (as was done in the JUPITER study), the individual variations in hs-CRP testing are less significant. There
is no doubt that it is a good predictor of cardiovascular risk for populations of patients. The concern, however is its usefulness
for an individual patient. The FDA panel today made it clear that there is no data showing treating to lower hs-CRP levels
is beneficial for patients, and it “did not allow for comparison between individuals with an hsCRP < 2 mg/L to those
with an hsCRP > 2 mg/L”. Crestor
is an excellent Statin medication for lowering LDL cholesterol, Triglycerides, along with Non-HDL cholesterol and Apolipoprotein
B levels. Its benefit in primary prevention, for BOTH men and women was well documented in the JUPITER trial. While hs-CRP
levels, if elevated over time may truly represent a patient at risk for cardiovascular disease, the patient and practitioner
should make sure to evaluate the complete picture. Smoking, Hypertension, Family History, Low HDL cholesterol and most importantly,
elevated APO-B containing lipoproteins, as measured by Non-HDL cholesterol, Apolipoprotein B levels, or LDL particle levels.
References 1.
Questions and Answers for Healthcare Professionals: CRESTOR and the JUPITER Trial
http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM199891 2. JUPITER Trial: Rosuvastatin
to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein N Engl J Med 2008 359: 2195-2207 3.
ApoB versus non-HDL-C: What to do when they disagree Current
Atherosclerosis Reports 2009, 11:358–363
Dr. Underberg
and Joe Theismann Discussing Aortic Aneurysm Screening Tackling AAA A bone-crunching
tackle prematurely ended the football career of former Washington Redskins quarterback Joe Theismann in November of 1985 in
a memorable game with the New York Giants. Voted the most shocking moment in NFL history, it was one that he, and many sports
fans, will never forget. But although he moved on to become a successful sports commentator and recently made a cameo appearance
in the new sports blockbuster movie, The Blind Side, Joe recalls another moment in his life that was just as shocking. It
was five years ago when his 89-year-old father, Joseph John Theismann, told him he’d been diagnosed with an aneurysm,
a bubble that forms in the artery that carries blood to and from the heart. “My dad told me he was ‘fine,’
not to worry,” Joe, a native of South River, N.J., recalls, “so I went along with it. I should’ve known
better.” Twenty-seven years before the aneurysm was diagnosed, Joe’s dad also had open-heart surgery.
And since then he’s had multiple stents implanted to open clogged arteries caused by atherosclerosis. “He was
fine then, too,” says Joe. “My father is that breed of human that says he’s fine no matter what’s
going on.” An eye-opening coincidence At that time, the high-profile sports commentator
and analyst also got a call from a group looking for a spokesperson to help get the word out about a little-known condition—abdominal
aortic aneurysm (AAA). The group, Find the AAAnswers (FindtheAAAnswers.org), wondered whether Joe knew
anyone with the condition. “I told them my dad had just been diagnosed with an aneurysm, but I didn’t
know if it was triple A,” he says. So he asked his father for the specific diagnosis—it was AAA. Joe
began learning about AAA, and realized how lucky his dad was to be alive. He became the group’s spokesperson, and began
urgently educating others about the condition through speeches, radio and television interviews, and other media appearances.
Why the urgency? According to Find the AAAnswers, about a million people in the U.S. are walking around with
the condition right now—and don’t know it. “My dad was one of those people,” Joe states.
People with AAA often don’t experience any noticeable symptoms, making the condition a silent killer and the third-largest
cause of death in men over 60 years of age. “If an aneurysm goes undetected, it can burst,” Joe explains, “and
you’ve got only a 10% chance of surviving.” Orange alert To make people more
aware of AAA, Joe often wears orange suspenders at TV and public appearances. “They’re a visual aid—they
cover the areas of the abdomen where these aneurysms occur,” he explains. Raising awareness is key to preventing sudden
deaths caused by ruptures. If AAA is detected early, doctors can prevent the bubble from bursting, typically by implanting
stents that not only unclog arteries, but also provide extra strength to weakened artery walls. Detection
is accomplished through an ultrasound, a painless procedure that takes about 10 minutes and lets the doctor see what is going
on in blood vessels. It can be done during a physical and men over the age of 60 should have it done annually. Most
men are happy to find out that the ultrasound doesn’t require special scheduling or preparation. “After all, at
one time, if I had a choice between going to a doctor’s appointment and playing a round of golf in the rain,”
Joe jokes, “I’d buy a wetsuit.” Now, however, he makes it a point to get an ultrasound at annual
checkups. The fit 62-year-old’s family history of heart disease puts him at higher risk for AAA. Both his father and
mother have atherosclerosis. And heart disease of any kind is a major risk factor. But risky behaviors, like smoking,
can also cause AAA (see “What Puts Me at Risk for AAA?”). “Smoking,” Joe stresses, “is
a big risk factor. My dad quit smoking almost 40 years ago, but it likely contributed to his condition.” Living
in Virginia with his third wife, Robin, Joe says he feels blessed. “My dad and mom are still with me in this world,”
he says. “That makes me a very lucky man.” When it comes to AAA, though, luck doesn’t apply.
“You have to take responsibility and make sure you get tested,” Joe concludes. “If you don’t, you
won’t really know if you have triple A.” And early detection ups your odds of survival to 95%, Joe notes. “Those
are really good odds.” How Is AAA Treated? The sooner AAA is detected,
the better. Early detection determines your best course of treatment, according to James A. Underberg, MD, clinical assistant
professor of medicine in the division of general internal medicine at New York University Medical School. Dr. Underberg specializes
in preventive cardiovascular medicine. “Treatment for AAA depends on the size of the aneurysm [a bubble
in the aortic artery]. If it’s small—between one to two inches—doctors watch it closely,” explains
Dr. Underberg. “We also recommend quitting smoking immediately, keeping blood pressure under control, lowering cholesterol
if it’s too high, and losing weight if you’re too heavy.” All of this helps to slow aneurysm growth. In
some cases, doctors also prescribe medication to reduce the blood pressure on the aneurysm. When an aneurysm is
larger than two inches, surgery is needed to remove it. Often, surgeons perform endoscopic vascular repair, which does not
require a large abdominal incision. Instead, a stent (a tube made of metal mesh) is inserted via catheters through the groin
and into the artery. The stent is secured in the abdominal aorta to support the weakened area of the artery. A
second option is open surgical repair. Surgeons create an incision and replace a section of the aorta with a tube. Recovery
from both procedures is fairly rapid, according to Dr. Underberg, and the likelihood of AAA recurrence is extremely low. —Kathy Gilligan Heart Care Health Monitor Winter
2010
|